Don't have an account?
Register NowYou have to add to cart at least 5 bottles or any program to make checkout.
- BlogWhat Is The Endocannabinoid System?
What Is The Endocannabinoid System?
Published: January 30th, 2023
Categories:
Medical Cannabis
It’s well-known that cannabis has powerful effects on people, but how exactly does it exert these effects?
The compounds found in cannabis are actually fairly similar to certain chemicals that are produced naturally in our bodies, and it is because of this that they are able to affect us in manifold, interesting ways.
In this article, we explore the endocannabinoid system—the system via which cannabinoids are able to affect how we think and feel.
What Is the Endocannabinoid System?
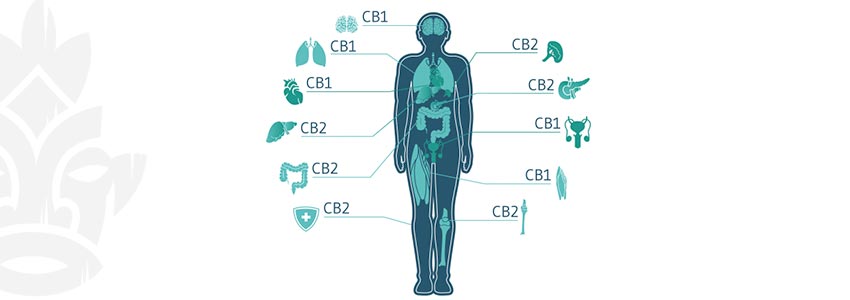
The endocannabinoid system (ECS) runs throughout the entire body. Found in the nervous system, brain, immune cells, organs, and more, this network of channels and receptors is responsible for cell signalling—i.e. informing cells of changes, and telling neurotransmitters to increase or decrease activity.
The full workings of the ECS are little understood, with the first cannabinoid receptor (CB1) discovered in 1988 by Allyn Howlett and William Devane. This receptor was found in the brains of rats, and then later, humans. In 1992, the discovery was made that there was in fact an entire network of receptors running throughout the body, which came to be named the endocannabinoid system. And in 1993, the second cannabinoid receptor was discovered.
Simply put, the ECS is chiefly composed of receptors, neurotransmitters (called endocannabinoids), and enzymes. The main receptors are CB1 and CB2, though some scientists have begun to deem TRPV1 the “CB3” receptor.
Anandamide (AEA), also known as the bliss molecule, is one of the main endocannabinoid neurotransmitters. AEA is an agonist of the CB1 receptor, and a partial agonist of the CB2 receptor.
The second endocannabinoid is 2-arachidonoylglycerol (2-AG). 2-AG is found in greater abundance in mammalian brains compared to AEA, and is a full agonist of both the CB1 and CB2 receptors.
There are four other compounds that are also suspected of being endocannabinoids:
- 2-Arachidonyl glyceryl ether (noladin ether)
- N-Arachidonoyl dopamine (NADA)
- Virodhamine (OAE)
- Lysophosphatidylinositol (LPI)
What Is the Function of the ECS?
The exact roles of endocannabinoids are not known, although it’s suspected that they influence a wide range of different functions and processes, including (but not limited to):
- Sleep
- Pain
- Inflammation
- Immune response
- Stress
- Fertility
What is highly suspected is that the ECS helps to maintain homeostasis—i.e. the dynamic equilibrium that keeps the body and its systems functioning. Specifically, the ECS is thought to support homeostasis by helping to balance hormone levels, immunity, body temperature, and much more. As such, the ECS appears to be a truly essential regulatory system.
How Do Cannabinoids Interact With the Endocannabinoid System?

Phytocannabinoids—those found in cannabis—were discovered before the ECS. In fact, the ECS was named after them, as the system was discovered as a consequence of research into cannabis.
The interactions between phytocannabinoids and the ECS are complex and, in some cases, little understood. In this section, we will explore how some of the better-understood cannabinoids interact with the ECS, and thereby exert effects upon the human mind and body.
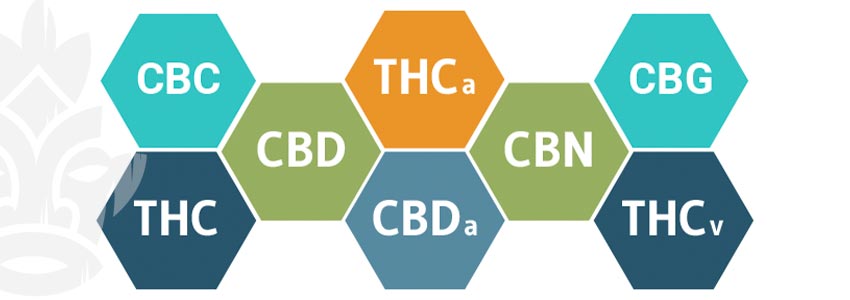
There are thought to be around 120 different cannabinoids produced in cannabis plants. Of these, we understand a fair amount about THC, enough about CBD to speculate, and very little about any of the other 118 or so.
That being said, research is growing at pace, and we now know some basic properties and mechanisms of certain cannabinoids, even if we are a far cry from saying with confidence if and how they may be used to benefit humans. Furthermore, it’s important to note that many cannabinoids are believed to interact with receptors outside of the ECS; therefore, the full scope of their mechanism of action is far from clear.
THC
Delta-9-tetrahydrocannabinol (THC) is the molecule that aided in the discovery of the ECS. For those who don’t know, THC is the intoxicating compound in cannabis that is responsible for causing a “high”. Until very recently, THC was the only cannabinoid that most people knew or cared about, but that is now gradually changing.
It is known that THC is a partial agonist of both CB1 and CB2 receptors. THC works primarily by mimicking the endocannabinoid AEA and binding to CB1 receptors in the brain. However, the body is able to break AEA down fairly easily, whereas THC is much more difficult for the body to metabolise. As a consequence, it causes a powerful high, and can also cause negative effects too, such as paranoia and anxiety.
Alongside its psychotropic influence, THC also interacts with CB1 and CB2 receptors in other parts of the body to produce a range of effects that may impact functions like appetite, sleep, and mood.
CBD
Cannabidiol (CBD) rose to prominence in the 2010s, and interest in the compound is only growing. Unlike its intoxicating sibling THC, CBD does not cause a high. But that doesn’t mean that it is without effects.
Though research is in its infancy, it is thought that CBD may be able to influence sleep, pain, inflammation, stress, anxiety, appetite, and more through its diverse mechanisms of action. Research posits that, in addition to the ECS, CBD interfaces with a range of other molecular targets, including serotonin receptors. As a consequence, there is now a huge amount of scientific research being conducted into CBD’s clinical potential.
What we do know is that, unlike THC or AEA, CBD does not bind to CB1 or CB2 receptors with much affinity. In fact, it may even partially block them. For this reason, it is thought that CBD may even have some potential to counteract the psychotropic effects of THC.
Another way that CBD is thought to work is by indirectly increasing concentrations of AEA. It does not stimulate AEA production outright, but rather inhibits its breakdown. There are two potential causes for this. The first is that CBD may inhibit FAAH, a fatty acid enzyme responsible for the breakdown of AEA. The second is that it might inhibit fatty acid binding proteins (FABPs), which transport AEA to FAAH to be broken down. In either case, what is fairly clear is that CBD increases anandamide concentration, and may therefore augment or extend the effects of AEA in the body.
THCV

Tetrahydrocannabivarin (THCV) is only present in trace amounts in most cannabis plants, though some breeders are trying to create cultivar that express higher levels of the cannabinoid. The reason for this is that, unlike most cannabinoids, it is thought that THCV may exhibit psychotropic properties. There are claims that THCV binds with CB1 receptors and causes a much more "clear-headed" high compared to THC. However, there is also research that refutes claims about THCV’s psychoactive properties.
Clinical research into THCV is difficult to conduct as it is present in such small amounts in most cannabis samples. In order to test it, huge quantities of cannabis flower must be processed to isolate enough THCV to give to participants.
CBN
Cannabinol (CBN) is created when THC breaks down. This can happen when buds are left on the plant after the optimal harvest date, or if the buds are improperly dried and cured post-harvest.
While not thought to be psychotropic on its own, CBN is believed to have notable effects, at least when taken alongside THC. Also interfacing with the CB1 receptor, though as a weak agonist, it is suspected that CBN causes a more lethargic high compared to THC alone—although this is yet unproven.
CBC
We know very little about cannabichromene (CBC). What we do know is that it is non-intoxicating and doesn’t appear to bind to CB1 or CB2 receptors. Instead, it appears to interact with the so-called “expanded ECS” via the TRPV1 and TRPA1 receptors. It seems likely that, via these mechanisms, CBC inhibits the body’s natural ability to break down the endocannabinoids AEA and 2-AG.
CBGA/CBG

Cannabigerolic acid (CBGA) is the original, so-called “mother”, cannabinoid. This is the very first cannabinoid to form in a young cannabis plant’s trichomes, and it is from this that all the others stem. By interacting with different enzymes, CBGA is biosynthesised into different “families” that in turn produce different sets of cannabinoids.
We know very little about what effects CBGA may have on its own. What we do know (or suspect) is that it interacts with both the CB1 and CB2 receptors, and the serotonin 5-HT1A receptors.
Other Compounds That Affect the ECS
Although cannabinoids bear most of the responsibility for the effects of cannabis, they do not work alone. Terpenes and flavonoids also have some impact on how cannabinoids interact with the body.
Myrcene, for instance, is a common terpene that gives cannabis (and mangoes) a peppery flavour and aroma. However, beyond just creating an interesting flavour, it is thought that myrcene might cause THC to cross the blood–brain barrier faster, thereby increasing the potency of the high.
This is just one example of a possible phytochemical synergy—commonly deemed the “entourage effect”—that occurs when numerous cannabis-derived compounds are consumed together.
The interactions between cannabinoids, terpenes, and flavonoids are yet another area that is woefully under-researched. But it is likely that, in time, we will know more.
The Endocannabinoid System: A Fascinating Enigma
The ECS is clearly a crucial system in the human body, but, as yet, we really have a very limited understanding of exactly what it does, and how we can influence it. Even where we do know how to influence it, we’re still a long way off being able to effectively target particular conditions with the correct concentrations of certain cannabinoids, for example.
Nevertheless, as cannabis legislation relaxes around the world and researchers have greater access to cannabis samples, we can be hopeful that we’ll soon understand more.